Forty-four-year-old Echo had always been the picture of health—active, ambitious, and ready to take on the world. But when unexplained symptoms began to disrupt her vibrant life, she found herself in a relentless quest for answers. Despite visits to prominent specialists who dismissed her symptoms as weight gain and “all in her head”, Echo knew something deeper was amiss. With each wave of pain, her determination grew stronger. She refused to accept that her suffering was a figment of her imagination. Driven by an unwavering belief that she deserved to be heard, Echo embarked on a journey that would lead her the experts at The Vascular Care Group and reveal the hidden truth of her condition—an arteriovenous malformation (AVM). Her story is a testament to resilience and the power of advocating for one’s own health in the face of doubt.
Echo was born in Georgia and relocated to Connecticut in 2021. Working as a grant administrator for a university, helping scientists submit research proposals, she enjoyed the adventure of living in several states and overseas as well.
 The tale of Echo’s hidden health battle began in 2016 when she was first diagnosed. “I was having severe bleeding, back spasms, and trouble with my urinary tract. My condition presented as a bladder tumor with gross hematuria. I had felt a mass in my abdomen, but a doctor said I was just gaining weight.” When she finally started bleeding and had a CT at the emergency department, she was referred to a urologist. The urologist attempted to biopsy the mass, but due to excessive bleeding, he had to terminate the procedure. He had no idea at the time that the mass was made of blood vessels. He sent Echo to Atlanta for a higher level of care, but the doctors there also struggled to understand her condition.
The tale of Echo’s hidden health battle began in 2016 when she was first diagnosed. “I was having severe bleeding, back spasms, and trouble with my urinary tract. My condition presented as a bladder tumor with gross hematuria. I had felt a mass in my abdomen, but a doctor said I was just gaining weight.” When she finally started bleeding and had a CT at the emergency department, she was referred to a urologist. The urologist attempted to biopsy the mass, but due to excessive bleeding, he had to terminate the procedure. He had no idea at the time that the mass was made of blood vessels. He sent Echo to Atlanta for a higher level of care, but the doctors there also struggled to understand her condition.
Between 2016 and 2020 Echo was being treated in Georgia and North Carolina. After her treating physician left the Emory system, she would drive five hours to continue with him. Unfortunately, during this time, she was misdiagnosed with a venous malformation (VM). She was told by both urology and interventional radiology that she could not be experiencing severe pain and pressure because the blood flow was not arterial.
In late 2023, Echo found Dr. Naiem Nassiri purely by chance. “I used to work at Yale and thought maybe Yale could help me. The first doctor said there was nothing that could be done, and I should just be happy that I didn’t have a hole in my organs from too many procedures, plus lots of other scary admonishments to just leave it alone because it was in too risky a location. I was so desperate and depressed from lack of care that I ended up choosing Dr. Nassiri at random.” Echo initially saw Dr. Nassiri at Yale but, as she explains, “I am very happy he is with The Vascular Care Group because he has more control over the procedures now, and I also like the level of care the staff provides at The Vascular Care Group.”
Echo’s story, while rare in its content, is not an unfamiliar one. All too often many vascular conditions go undiagnosed or misdiagnosed by well-meaning clinicians who lack the specialized experienced possessed by board-certified vascular surgeons. Echo tells it best:
“It’s difficult to describe how I felt the mass inside me for the past eight years of failed treatments—and even for years before my diagnosis. I felt its pressure in my pelvis; it hurt to sit. I felt tingling and other nerve pain down my right leg and into my foot all the time, and especially after any form of exercise. It felt almost like I had a peg leg, like my right leg was not my own. I could feel where the mass touched my female organs. It was very painful. Sometimes the pain was so bad I felt like I did not want to live. It felt hopeless. Other people sometimes made fun of me for being out of shape because on the outside, I looked normal. It was embarrassing for people to treat me like I was lazy for not doing cardio when in fact cardio was excruciating.
During my treatment, I also went into early menopause in my 30’s and had no idea it was happening to me. I do not know if it is related to the pelvic AVM. To date, I’ve had 11 operations. Some doctors suggested the embolization may have killed my ovaries, but I suppose I will never know. I did not have children before this happened, so we have a dog and cats instead. I struggled with my mental health. Having an AVM in your pelvis is enough without also losing your sense of womanhood.
“I knew from the type of pain I was feeling in the week after surgery that something had changed for the better. The last procedure I’d had that reduced my symptoms was on the arterial side in 2017. At that time, my previous doctor was very aggressive, trying to close off the mass with coils and glue without success. However, it seemed like he backed off after that due to some post-surgery severe issues I had with my bladder.”
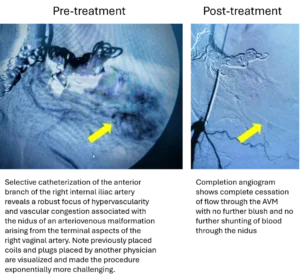 Echo underwent two procedures, one in June on the venous side and another in July on the arterial side of the mass, targeting the nidus. Dr. Nassiri was able to micro-catheterize the vaginal branch of the right internal iliac artery anterior branch and embolize the AVM nidus with glue, achieving excellent deposition. There was no evidence of any non-targeted embolization. The completion angiogram demonstrated successful obliteration of the AVM nidus. Each of the procedures were able to be performed in the ambulatory setting, and Echo was able to return home the same day.
Echo underwent two procedures, one in June on the venous side and another in July on the arterial side of the mass, targeting the nidus. Dr. Nassiri was able to micro-catheterize the vaginal branch of the right internal iliac artery anterior branch and embolize the AVM nidus with glue, achieving excellent deposition. There was no evidence of any non-targeted embolization. The completion angiogram demonstrated successful obliteration of the AVM nidus. Each of the procedures were able to be performed in the ambulatory setting, and Echo was able to return home the same day.
“Three weeks out from surgery with Dr. Nassiri, the pain has abated, and I feel a dramatic reduction—heck, an elimination—of the pain in my pelvis. I feel cured, which is the word Dr. Nassiri used when I saw him for my post-op visit. Being cured of a persistent AVM feels like a miracle. Dr. Nassiri took calculated risks to put glue into the nidus, or origin, of the mass, which is like its control center. Because he reached the nidus, I can have faith that it will not grow back.
Having a mass made of blood vessels presents unique challenges because 1) it can find new blood sources and grow back (as it has many times), and 2) surgeons can’t just excise it. Throughout this hidden battle, many doctors refused to even see me—not only surgeons, but also gynecological and primary care doctors who found my situation too “risky” and would tell me things like I was going to bleed to death. After I started randomly bleeding following some physical activity in 2024, I packed a hospital bag, almost like having a bag you would have ready for having a baby, in case I hemorrhaged at home.”
Now three months later, Echo says she is still working to build her energy level back to normal and still has some lingering pain, but not much. Most importantly, she says, “I no longer have any pressure in my pelvis. I recently enjoyed a trip to downtown New Haven and the Beinecke Rare Book and Manuscript Library without wondering if I would be in severe pain after walking.”
At her recent follow up visit after two sessions of embolization, Echo states that she finally feels essentially normal. She has had no further bleeding and is exercising now, which she has not been able to do in many years. She is very pleased with the results.
We asked Echo to share her story in case it helps other women. She wants to share these final thoughts on her hidden battle and her experience with The Vascular Care Group.
“Having a vaginal AVM is a rare condition, and it is difficult to find resources online. I would say, for anyone who is not seeing results from their treatments or anyone who doesn’t know where to turn, that Dr. Nassiri has the skill and expertise to get the job done. Dr. Nassiri validated my experience. He told me the pain and pressure I’d felt were real. He told me I was misdiagnosed and that he was glad I listened to my body. After years of male doctors telling me I was not in pain and didn’t have an AVM, I felt comforted and liberated.
I would encourage any woman struggling with a vascular issue to seek a consult with The Vascular Care Group. I would especially encourage women with a pelvic AVM to contact Dr. Nassiri. He is not just a surgeon; he is also a researcher and scientist. He runs clinical trials. He is a real expert on this condition.”
From the onset of her complications in 2016 until the completion of her treatments in 2024, she has had quite an extraordinary journey, and we are proud that our team played an integral role in ultimately restoring her quality of life.
