The vascular anomalies and malformations program, TVCG CARES International, at The Vascular Care Group, is a highly specialized program providing management of all vascular anomalies including hemangiomas and vascular malformations.
At TVCG CARES, we provide comprehensive, state-of-the-art, multi-disciplinary diagnostic and therapeutic services for patients with vascular anomalies. We also aim to increase patient, community, and physician awareness about vascular anomalies and malformations throughout New England and beyond.
The CARES team provides a coordinated treatment plan tailored to each patient’s specific problem. We aim to educate patients and their families such that a realistic expectation of the course of the disease as well as treatment outcomes exists. As mentioned, treatment options are broad requiring the expertise of many different specialists each with unique sets of skills and experience.
These include surgical resection and reconstruction, catheter-based techniques such as embolization and sclerotherapy, laser therapy, medical therapy, and simple observation with regular follow-up. Often, a combination of these methods is necessary for optimal results. The CARES team meets on a regular basis to discuss every patient’s case individually. Options are discussed and the safest, most appropriate treatment plan is chosen and offered considering all possible risks and benefits. https://tvcgcaresinternational.com
Conditions We Treat
Below are examples of some of the more common conditions we treat:
Hemangiomas
Infantile Hemangiomas
These are by far the most common type of hemangioma and resemble most closely the classic “strawberry birthmark” you may have seen or heard of. They are occasionally present at birth but most commonly do not become noticeable until about 2 weeks to 2 months after birth. While there are many theories out there regarding the cause of hemangiomas, the simple answer is that we do not know what causes hemangiomas; at least, not yet. We do know that they are more common among Caucasian females of low-birth weight.
Infantile hemangiomas tend to occur more commonly on the head and neck area. The skin is by far the organ most involved, so most of these lesions are readily identifiable. If the hemangioma is located near a vital organ such as the airway or the eye, a much more aggressive treatment approach is sought to prevent problems with organ and functional development. Infantile hemangiomas can also involve the organs inside the body such as the liver, intestines, or the airway occasionally in conjunction with a hemangioma of the skin. These are much more difficult to identify and diagnose and can sometimes be an incidental discovery. Most, not all, internal hemangiomas tend to be problematic and are treated aggressively.
Regardless of location and severity of symptoms, true infantile hemangiomas have a characteristic and predictable pattern of presentation and regression. They are typically identified around 2 weeks to 2 months after birth and grow until about 12 months of age. This growth period is called the “proliferation phase”. Thereafter, they undergo a long, drawn-out n involution phase which occurs from about 12 months of age and can last until about adolescence and the pre-pubertal period. This period is termed the “involution period”. From there on out, there is continued remodeling and scarring of the residual components of the hemangioma. This period is called the “involuted period”.
The key component in management of any infantile hemangioma is early referral and evaluation at a dedicated center of excellence with a multidisciplinary approach. Earlier intervention can minimize and correct potentially serious problems during the proliferation phase (such as visual, respiratory, or digestive problems). It has also been effective at reducing the need for extensive surgery late in the involution or involuted periods. It also minimizes the inherent psychosocial complications associated with a disfiguring, readily apparent lesion.
Available treatment options include simple observation, pharmacotherapy (steroids, beta-blockers, and/or immunomodulators), surgical excision with reconstruction, laser therapy, and rarely catheter-directed techniques such as angiography with or without embolization (injection of different types of particles directly into the problematic area to eliminate or reduce its blood supply). Often, a combination of these techniques is required for optimal results.
Congenital Hemangiomas
These are much rarer hemangiomas and have a different pattern of presentation than the classic infantile hemangiomas. They have a predilection for the upper trunk and the extremities (arms and legs). Unlike infantile hemangiomas, they are present at birth (congenital) and either undergo rapid (within 6-12 months) regression (termed rapidly involuting congenital hemangioma or RICH) or do not regress at all (termed non-involuting congenital hemangiomas or NICH). Treatment for these is variable depending on location and associated symptomatology. Like infantile hemangiomas, early referral to a dedicated center of excellence is key in eliminating or minimizing associated complications.
Kaposiform Hemangioendothelioma / Tufted Angioma
These are extremely rare hemangiomas that have a much more aggressive pattern of growth and can invade multiple tissue planes or layers of the body. Given their aggressive nature, they can be associated with consumption of the body’s own inherent clotting mechanisms and can lead to potentially serious and sometimes lethal bleeding and clotting complications. This serious complication is termed Kasabach-Merritt Phenomenon – a condition that deserves immediate medical attention. Again, we emphasize early referral to and evaluation by a dedicated center of excellence to minimize potentially lethal consequences.
Vascular Malformations
Capillary Malformations (Port-Wine Stains)
One can think of these as a vascular malformation of the tiniest blood vessels in the body occurring in the most superficial layer of viable skin, called the dermis layer. They are a deep red to purple in color and can occur anywhere on the body. Like all other vascular malformations, these are present at birth and tend to grow throughout the lifetime of the patient with thickening of the affected portion of the skin and darkening of the primary color. These changes are partially attributable to the chronic local inflammatory changes that take place because of the malformation.
Capillary malformations can either be isolated or associated with other, more extensive syndromes, particularly when a specific pattern of distribution is noted. Syndromes associated with capillary malformations include Klippel-Trenaunay Syndrome, Parkes-Weber Syndrome, and Sturge-Weber Syndrome. In these cases, a dedicated search to identify vascular malformations in other organs is necessary to prevent potentially devastating complications of untreated lesions.
The first line of treatment for problematic capillary malformations is laser therapy via a pulsed dye laser. Multiple treatments are often needed. Results vary depending on the location of the malformation with the general rule of thumb being those central lesions (face, head, neck) fare better than more peripheral lesions (hands and feet). Early treatment is encouraged to optimize results prior to more extensive chronic local inflammatory changes taking place. These are relatively well-tolerated with minimal complications, the most common of which is scarring from multiple treatments. As with all other vascular malformations, there is no cure for capillary malformations and recurrence is not an uncommon event. Treatment does not eliminate the lesion completely. In other words, laser therapy will not eliminate the associated discoloration, but significant improvement is frequently achieved. Regular follow-up at designated intervals is required for optimal maintenance of therapy.
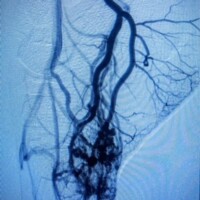
Slow-Flow Venous Malformations
Veins are blood vessels that carry blood from organs back into the heart and lungs for re-oxygenation. Under normal circumstances, venous circulation is a low-pressure system. Malformations affecting the venous circulation are, by far, the most common comprising nearly 75% of all vascular malformations. Venous malformations can either be isolated or part of a syndrome, most commonly Klippel-Trenaunay Syndrome. The cause is unknown although certain genetic mutations have been identified in patients with these malformations. Venous malformations can either be an isolated event in an individual sporadically or inherited from parents in a familial form. They are present at birth but do not become apparent until later in life when an external or internal stimulus such as activity, injury, puberty, pregnancy, surgery, etc. triggers symptomatic exacerbation of the malformation. They can happen anywhere in the body at any depth. Symptoms range from minor aches and pains to recurrent, life-threatening hemorrhage, clotting disorders, and organ damage, mostly within bones, joints, and skeletal muscles.
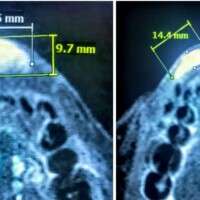
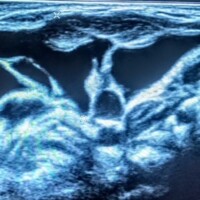
These lesions are readily identified on properly conducted MRI studies. Treatment primarily consists of Direct Stick Embolization under ultrasound or x-ray. This treatment is generally well-tolerated if performed judiciously with focal treatments performed in multiple sessions dispersed over several sessions with appropriate length intervals in between sessions. Aggressive treatment of large areas can cause local skin and nerve damage, and heart and lung related problems.
Surgery is not an ideal first-line therapy for these lesions given the risk for bleeding and disfiguring results following resection of involved tissue planes. Surgery can, however, be very effective when performed in conjunction with sclerotherapy. This concept emphasizes the importance of close collaboration among treating physicians from various specialties. Moreover, Dr. Naiem Nassiri who has extensive training and expertise in both open surgery as well as minimally invasive, endovascular, and interventional techniques. As a result, the most appropriate and effective treatment or combination of treatments is offered to the patient without limitation.
As with all other vascular malformations, treatment is geared towards controlling and minimizing symptoms. There is no absolute cure for these lesions. Multiple treatments are often necessary and recurrence is not uncommon. In general, focal, superficial lesions are more effectively treated than widespread, deep lesions.
Slow-Flow Lymphatic Malformations
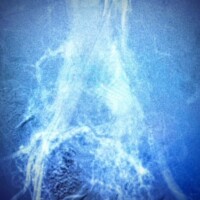
Lymphatic vessels are channels that carry fluid existing outside of blood vessels (arteries and veins) back into the blood circulation. Like veins, they function in a low-pressure environment under normal circumstances. Malformations affecting the lymphatic channels can be secondary to an obstruction or a congenital deformity of the walls of the lymphatic channels themselves. This results in stagnant lymphatic flow and pooling of the lymph fluid into cysts or fluid-filled pockets of various sizes. These cysts can be bled into, become infected, or both. If large enough, they can cause problems by impinging upon and compromising the function of adjacent organs such as the aerodigestive tract. The limbs such as the legs and feet can also be affected although these can have variable patterns and timing of presentation.
Lymphatic malformations are congenital (present at birth). But unlike venous malformations or arteriovenous malformations, they manifest much earlier in life, during infancy and early childhood because they are not as hormonally regulated as blood vessels are.
Diagnosis is made by ultrasound, MRI, and rarely CT scans depending on location and pattern of presentation. Most commonly, the first-line treatment is drainage of the cysts by a catheter followed by injection of the drained cyst cavity with a sclerosant (a detergent-like compound that causes irritation, inflammation, and gradual collapse of lymphatic cyst). This is most successful for larger cysts (those greater than 2 cm). Smaller cysts, called microcysts, are more difficult to treat. Multiple treatment sessions may be required, and recurrence is not uncommon.
Surgery as first-line treatment is generally not recommended as complication rates can be high. Surgery is best reserved for residual lesions after sclerotherapy or for smaller cysts not responding to sclerotherapy.
Laser therapy can also be offered for specific types of lymphatic malformations and their associated overlying skin changes.
High-Flow Arteriovenous Malformations
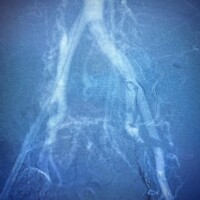
Arteriovenous malformations represent an abnormal connection between arteries (blood vessels that supply the body organs) and veins (blood vessels that drain the body organ). One can think of this as a short-circuit of sorts wherein blood pumped from the heart to a given organ is prematurely redirected away from that organ back towards the heart. This can create a vicious cycle of abnormal blood flow that deprives the affected organ from oxygen and nutrients and can take a toll on the circulatory system including the heart and the affected blood vessels. If severe enough, it can cause heart and/or organ failure.
As with all other vascular malformations, arteriovenous malformations are present at birth (congenital) but do not become problematic until later on in life as the malformation continues to grow with the patient and becomes affected by changes in the hormonal environment as well as activity and/or local trauma. By far, the most important factor in management of arteriovenous malformations is early detection and treatment.
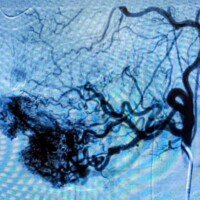
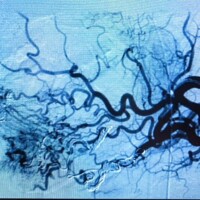
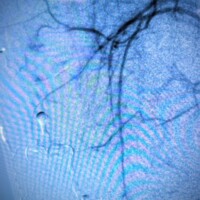
Congenital arteriovenous malformations can be present anywhere in the body but have a predilection for the brain, spinal cord, and the extremities. Rarely arteriovenous malformations of the internal organs such as the kidneys, the intestines, and the lungs can be detected. Early referral to a dedicated center of excellence is key. Diagnosis will inevitably depend on a series of imaging studies such as ultrasound, MRI, and angiography. Treatment is almost always indicated to minimize symptoms and decrease the likelihood of expansion and organ loss. In some rare cases, the malformation has expanded severely enough such that treatment may provide little to no benefit and management is geared more towards palliation of associated symptoms.
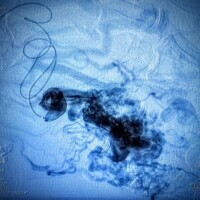
The mainstay of treatment for arteriovenous malformation is catheter-based embolization. The term embolization refers to delivery of certain particles or substances as closely as possible into the focus of the arteriovenous malformation. These particles or substances will then act to shut down the malformation by disrupting the blood supply to the focus of the malformation and redirecting blood flow back into the normal circulation. Most commonly, multiple treatment sessions will be required throughout the lifetime of the patient. It is important to emphasize that there is no cure for arteriovenous malformations and that treatment is aimed at minimizing symptoms and slowing the progression of the disease. Even with successful treatment, certain severe cases can continue to expand and cause organ and/or life-threatening problems.
Surgery by and large is not recommended as primary treatment of arteriovenous malformations except in rare refractory cases or to treat associated complications of the malformation.

Congenital Mixed Syndromes
Klippel-Trenaunay Syndrome (KTS)
Klippel-Trenaunay Syndrome or Klippel-Trenaunay-Weber Syndrome or KTS refers to the triad of port-wine stains, bony and/or soft tissue overgrowth, and slow-flow venous / lymphatic malformations. The diagnosis is made if 2 of these 3 criteria are present. The cause is unknown.
The venous malformations in KTS can be quite extensive and involve bones, joints, muscles, as well as the skin and the underlying fat. The major veins of the limb themselves can also have issues with reflux and cause pooling of blood and fluids into an already overgrown limb. This leads to high pressures within the compartments of the limb and increases the likelihood of debilitating pain particularly with walking or prolonged standing. Furthermore, there is an increased risk of recurrent infections as well as clotting of the veins. Ulcerations and skin sloughing because of these very high pressures are also not uncommon.
The mainstay of treatment for KTS remains appropriate grade compression stockings and limb elevation. Direct-stick embolization of the underlying venous malformation can be performed in multiple sessions. This can help reduce symptoms significantly. Laser therapy is also available for the port-wine stain component. However, what can be most helpful is addressing the major vein trunks that run superficially along the limb. Previously, it was thought that patients with KTS have an underdeveloped or absent deep vein system. As a result, treating or ablating the superficial veins of the limb was deemed inappropriate and detrimental. It has been shown that many patients with KTS do, in fact, have a functioning, open deep system. This must be delineated and identified appropriately with newer diagnostic modalities that are ultrasound-based. As a result, treatment of the more superficial components of the venous system in patients with KTS ca be safely performed with significant improvement in symptoms.
Parkes-Weber Syndrome
This is very similar to Klippel-Trenaunay Syndrome with the exception that instead of the slow-flow venous malformations of KTS, there are high-flow arteriovenous malformations associated with the limb. Treatment is primarily catheter-based as with other high-flow arteriovenous malformations.
Blue Rubber Bleb Nevus Syndrome
Also known as Bean Syndrome, this refers to presence of multiple, widespread foci of isolated slow-flow venous malformations dispersed throughout the skin and underlying tissue as well as the intestines, and the internal organs. Refractory bleeding is a concern, so endoscopy is often necessary. Direct stick embolization in conjunction with surgical excision can address the most symptomatic skin and soft tissue lesions. More extensive surgery may be necessary for internal bleeding that does not respond to endoscopic intervention.
CLOVES Syndrome
CLOVES is a mnemonic that refers to Congenital Lipomatous Overgrowth, Vascular malformations, Epidermal nevi, and spine deformities. It is a disease of infants and young children. It features fatty tissue overgrowth throughout the body sparing the head and neck. The feet and limbs are very commonly affected as well as the trunk. Multiple foci of venous and/or lymphatic malformations are present. A characteristic red-purple rash called epidermal nevus is also identified. A component of this may be simply a port-wine stain representing a capillary malformation. Furthermore, spinal deformities such as scoliosis and high-flow arteriovenous malformations affecting the spinal cord are detected.
The cause is unknown, and treatment is mostly palliative. Treatment approach is truly multidisciplinary requiring the expertise of many physicians including vascular interventionalists, orthopedic surgeons, plastic surgeons, pediatric surgeons, pediatric hematologists, and neurosurgeons and neurointerventonalists.
Hereditary Hemorrhagic Telangiectasias (HHT)
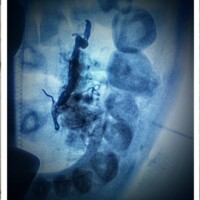
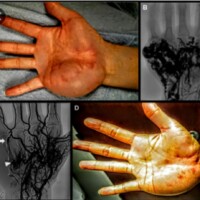
HHT or Osler-Weber-Rendu Syndrome refers to malformations of small end arteries which can lead to formation of tiny arteriovenous malformations affecting the skin, internal organs, aerodigestive tract including the mouth, nose, and lungs. This is a hereditary disorder which is passed down from parents to children. The presenting signs include multiple nosebleeds, skin rash particularly on the palms of hands and feet, and presence of arteriovenous malformations within the internal organs.
One of the most serious complications associated with HHT is the presence of arteriovenous malformations within the pulmonary circulation. These can by asymptomatic or present with bloody cough. Nevertheless, treatment is almost always necessary as clots from the limbs can be shunted through this malformation and wind up in the brain. Once in the brain, the clot can have devastating complications including stroke and infection with formation of a brain abscess. Embolization of these pulmonary malformations is, therefore, highly recommended.