What is Carotid Artery Disease?
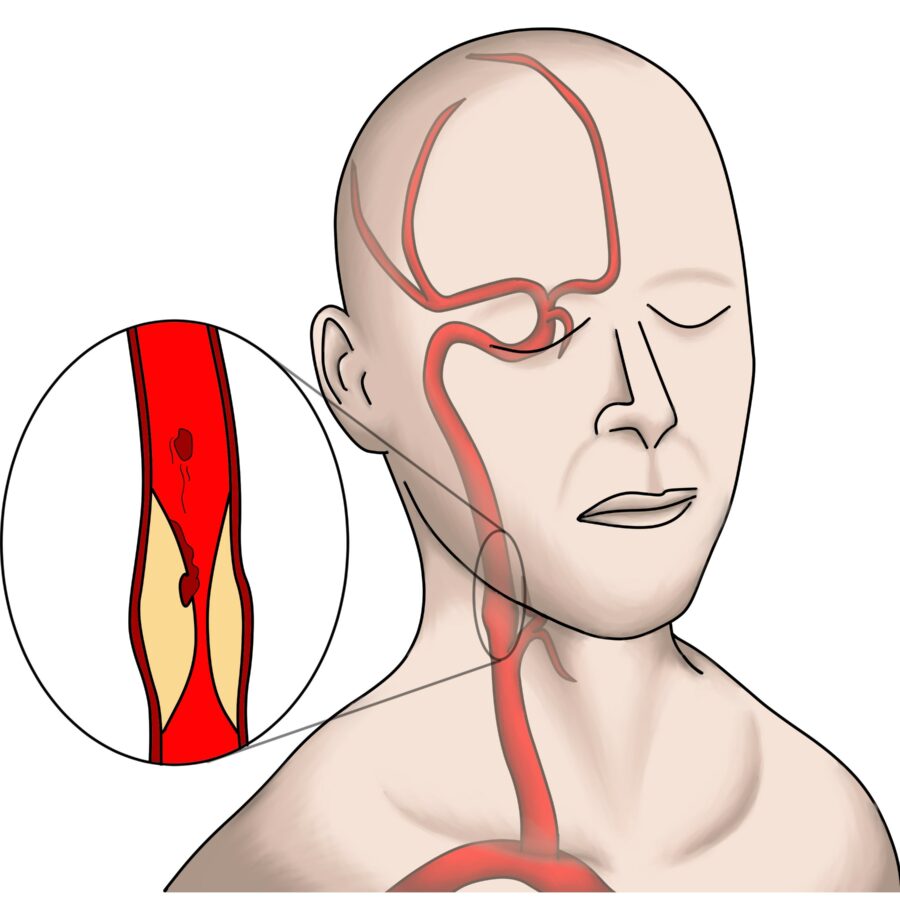
Your carotid arteries are the two main arteries that carry blood from your heart, up through your neck, to your brain. Healthy carotid arteries are smooth and unobstructed, allowing blood to flow freely to the brain and providing oxygen, glucose, and other nutrients that your brain cells need.
Typically, with age, the carotid arteries build up plaque, made up mostly of fat and cholesterol. Plaque narrows the inside of the arteries and makes them stiff. This process is commonly referred to as “hardening of the arteries,” or atherosclerosis and is the same process that causes coronary artery disease and heart attacks.
Carotid artery disease results when the carotid arteries become narrow or obstructed and create a risk of the plaque traveling to the brain and causing a stroke. This risk increases the more the artery narrows.
Stroke is the third leading cause of death in the United States and the leading cause of permanent disability in older adults. Approximately 25% of strokes occur when bits of carotid plaque or clot break off and flow to the brain.
If left untreated, carotid artery disease may lead to stroke, where the lack of oxygen and other essential nutrients cause damage to the brain. Depending on its severity, a stroke can be permanently disabling or even fatal.
Risk Factors
Know your risk for Carotid Artery Disease
Anyone can develop carotid artery disease, but there are certain risk factors that can increase the likelihood of developing this serious condition.
These conditions include:
- Smoking
- Age
- High blood pressure
- Diabetes
- High cholesterol
- Obesity
- Lack of exercise
- Family history of atherosclerosis and/or stroke
Symptoms of Carotid Artery Disease
There may be no symptoms in the early stages, and stroke could be the first sign of the condition.
A stroke has warning signs. These are referred to as mini-strokes or transient ischemic attacks (TIA’s).
Mini-stroke symptoms are usually temporary, lasting a few minutes to a few hours, and should be treated as serious medical emergencies requiring immediate treatment, as they are strong predictors of future stroke.
Some symptoms of stroke or TIA may include:
- Weakness, numbness, or tingling on one side of the body.
- Inability to control movement of a body part.
- Loss of vision in one eye.
- Inability to speak clearly.
- Difficulty talking or comprehending what others are saying.
Diagnosing Carotid Disease
Your vascular provider will evaluate your medical and family history. Then they will do a thorough physical exam. If needed, a vascular ultrasound that we do in the office can confirm the presence and the severity of the disease.
If you experience symptoms of a ministroke or stroke, seek medical attention immediately. Your physician may then ask you to see a vascular surgeon to assess if a surgery is warranted.
What are the treatment options?
Depending on the severity of your condition, treatment options may include lifestyle changes, medications, or procedures such as carotid endarterectomy or carotid artery stenting. Vascular surgeons use two approaches to carotid artery surgery. The procedures are similar, but having both options enables your surgeon to choose the one that meets your particular needs.
Transcarotid Arterial Revascularization (TCAR)
Some patients also benefit from a newer, minimally invasive procedure producing excellent results and outcomes called TCAR.
TCAR is the placement of a stent across the area of stenosis. Although it requires a small incision in the neck, the recovery is faster with less pain and scarring then CEA.
TCAR takes place in an operating room. After you’re placed under anesthesia, the surgeon makes a small incision in your neck, just above the collarbone. A tube is placed directly into your carotid artery and then connected to a system that temporarily reverses blood flow away from the brain; this prevents any loose bits of plaque from reaching the brain and causing a stroke. (Your brain still receives adequate blood from other arteries.) The blood is filtered by the system and then returned to your body through a second tube connected to a vein in your groin. While the blood flow is reversed, a stent (a small, expandable tube) is inserted into the artery to stabilize the plaque and prevent it from causing strokes. After the stent is in place, the surgeon halts the blood flow reversal and your blood resumes flowing toward the brain.
More than 20,000 TCAR procedures have been performed in the United States, and the data on patient outcomes have been excellent.
Most patients can go home the day after the procedure and resume normal activities quickly. Recovery is faster than with traditional surgery, with minimal pain and less scarring.
You will probably be prescribed medications to prevent blood clots in your newly opened artery. It’s important to follow your doctor’s instructions for these medications. As part of your follow-up care, your doctor may order a later ultrasound to determine whether the stent is working.
Traditional carotid endarterectomy
Traditional carotid endarterectomy involves an incision along your carotid artery. It enables your surgeon to more easily use a shunt, a tube to keep blood flowing to your brain during surgery. The surgeon closes the artery with a patch from another blood vessel in your body or a synthetic or biologic material.