- Learn more about Genicular Artery Embolization
- Learn more about Uterine Fibroid Embolization
- Learn more about Rectal Artery Embolization
What are Uterine Fibroids?
Uterine fibroids (UF), or leiomyomas, are benign tumors arising from uterine smooth muscle. These growths develop in the uterus and appear alone or in groups. They range in size from as small as a grain of rice to as big as a melon. In some cases, fibroids can grow into the uterine cavity or outward from the uterus on stalks. An estimated 20% to 50% of women of reproductive age currently have fibroids, and up to 77% of women will develop fibroids sometime during their childbearing years. Only about one-third of these fibroids are large enough to be detected by a health care provider during a physical exam, so they are often undiagnosed. As UF grow in volume, symptoms including constipation, bladder dysfunction, and chronic back and pelvic pain



What are the Risk Factors?
The exact etiology of UF remains unclear. Research suggests each tumor develops from an abnormal muscle cell in the uterus and multiplies rapidly when encountering the estrogen hormone, which promotes the tumor’s growth.
Women in their reproductive age are most likely to be affected by fibroids.
Other risk factors may include:
- Family history of fibroids
- Obesity
- Diet high in red meat
- High blood pressure
Black women are more likely to develop fibroids than other women, they are diagnosed at younger ages, and more often require treatment. It is not understood why they are disproportionately affected. Bleeding and symptoms associated with UF tend to improve with menopause, suggesting that the persistence of UF depends on hormonal status. There is also a hereditary component, first degree relatives of women affected by UF having a 2.5 fold higher risk of developing UF.
Symptoms and Diagnosis
What are the Symptoms?
While some women with fibroids may not experience any noticeable symptoms, others commonly experience severe symptoms that interfere with their daily lives, such as:
- Heavy or prolonged periods
- Bleeding between periods
- Abdominal discomfort and/or fullness
- Pelvic pain
- Lower back pain
- Bladder symptoms, such as frequent urination or difficulty emptying the bladder
- Bowel symptoms, such as constipation or excessive straining with bowel movements
Women with fibroids can also experience:
- Infertility
- Complications during pregnancy
How are they Diagnosed?
Fibroids are most often found during a routine pelvic exam.
To diagnose uterine fibroids, your doctor may order one of the following tests:
- Pelvic Ultrasound. The doctor can see the size, shape, and texture of the uterus and evaluate any growths.
- Magnetic resonance imaging (MRI). Helps your provider determine the exact location and characteristics of fibroids.
- Hysterosalpingography. This is a to determine if the fibroids have blocked your fallopian tubes.
- Hysteroscopy. This is a visual exam of the canal
Treatment
What about the Treatment options?
The traditional approach to UF management has been surgical. Hysterectomy remains the predominant intervention, with myomectomy an option for women desiring to maximize fertility. Uterine artery embolization (UAE) is a minimally-invasive and uterine-preserving procedure that has become an attractive therapeutic alternative over the last 20 years. Its effectiveness and safety profile have helped establish this technique as a viable option with minimal complications for women interested in retaining their uterus and avoiding invasive surgery.
Tell me more about Uterine Fibroid Embolization?
UFE is a minimally-invasive alternative and/or adjunctive therapy to hysterectomy or myomectomy. This procedure is performed in our office and requires no hospital stay and offers a shorter recovery. In this procedure, blood supply to the fibroid tumors is blocked, making them shrink.
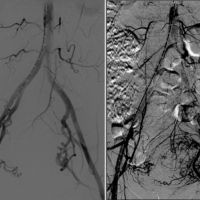
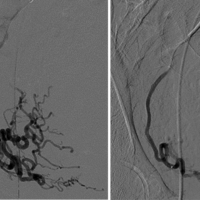
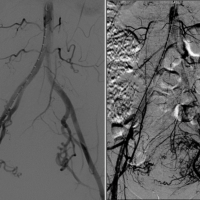
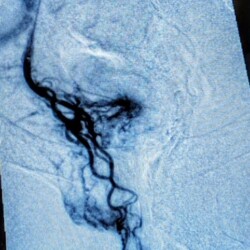
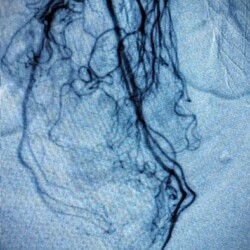
During UFE, a catheter is inserted through a blood vessel in the groin or arm and guided by X-ray images to the blood vessels that feed the fibroids of the uterus. Tiny particles are then injected to stop blood flow to the fibroids. Once blood flow to the fibroids is blocked, patients return home while the fibroids shrink gradually over the next weeks and months.
Uterine fibroid embolization is a very effective procedure with an approximate success rate of 85%. Most individuals who undergo the procedure have a dramatic improvement in their symptoms and a decrease in size of their uterine fibroids. If menstruation has been heavy, it will usually return to a more normal flow after UFE.
Fibroid embolization is a minimally invasive therapy that does not require surgery or a hospital stay and lessens recovery time compared to other treatments.
Some final thoughts
What can I Expect Following Embolization?
There are no restrictions after the procedure. It typically takes a week to 10 days to recover from embolization. In the first few days, pelvic pain and pressure from the procedure can be present. Fevers, chills, and decreased energy levels such as you would experience with a cold or flu can also be present. Your vascular surgeon will prescribe adequate pain, anti-inflammatory, and/or anti- nausea medication for use at home.
The first cycle following the procedure will frequently be heavier, with more discomfort than usual. Breakthrough bleeding in between menstrual cycles is common in the first few weeks. It typically takes 3 months for the benefits of the procedure to be appreciated, and the fibroids commonly continue to shrink for 6-9 months or longer.
Emborrhoid Technique of Superior Rectal Artery Embolization

Hemorrhoids
What are Hemorrhoids?
Nearly half of adults over than 50 have hemorrhoids, which are swollen and enlarged veins in the anus or lower rectum. In addition to becoming more common with age, hemorrhoids may result from pregnancy, obesity, repeatedly lifting heavy weights, frequent constipation or diarrhea, or straining during bowel movements. Hemorrhoids are the most common anorectal disease.
Some hemorrhoids are external, in the area around the anus, and might cause itching, pain, discomfort and bleeding, while others are internal, in the rectum. Internal hemorrhoids can lead to bleeding during or after bowel movements; these hemorrhoids also may prolapse, or push through the anus, causing pain or irritation and bleeding.
Internal hemorrhoids are graded based on how much they protrude:
- Grade 1 hemorrhoids do not prolapse outside the anus.
- Grade 2 hemorrhoids protrude through the anus during straining or bowel movements but return to place on their own.
- Grade 3 hemorrhoids might have to be manually pushed back into place.
- Grade 4 hemorrhoids remain prolapsed outside the anus.
Some hemorrhoids go away on their own. You can treat hemorrhoids with topical medications and with high- fiber diets that promote soft stools, decreasing the need to strain during bowel movements. Prolapsed hemorrhoids and hemorrhoids that cause bleeding, however, often require medical treatment. Standard treatments include nonsurgical procedures that use banding around the hemorrhoids or cauterization of the hemorrhoids to cut off blood supply, and surgical removal for advanced hemorrhoids.
Symptoms and Benefits
What are the Symptoms?
- None – many people with hemorrhoids have no symptoms.
- Itching of the skin around the anus
- Bright red blood after using the toilet which is often painless
- Pain if a blood clot forms inside a hemorrhoid. In this case, you may also feel a lump
- Swelling of hemorrhoids outside of the rectum (prolapse) during a bowel movement
What are the Benefits of Embolization?
Minimally invasive: it is performed using a small needle puncture and does not require general anesthesia. This means no hospital stay and a faster recovery time than traditional surgery. It also does not require any bowel prep.
High success rates: studies reporting success rates of up to 90%. This means that most patients experience significant improvement in their symptoms after the procedure.
Minimal pain and discomfort: compared to traditional surgery, and patients typically require only mild pain medication after the procedure.
Reduced risk of complications: lower risk of complications compared to traditional surgery, such as bleeding, infection, and incontinence.
Suitable for bleeding internal hemorrhoids: can be used to treat the majority of bleeding internal hemorrhoids, but tends to be more effective in low to moderate grade hemorrhoids without prolapse.
Outpatient procedure: can be performed as an outpatient procedure in our office, meaning patients can return home the same day.
Quick recovery time: most patients can return to their normal activities almost immediately, which is a vast improvement over traditional surgery.
Treatment
Are you a Candidate?
- You have pain from hemorrhoids
- You have bleeding from hemorrhoids
- You feel dilated veins in your anus
- Do not want surgery
What is the Emborrhoid Technique of Hemorrhoid Embolization?
Emborrhoid or Hemorrhoid embolization is an minimally invasive treatment for internal hemorrhoids that offers long-lasting relief from rectal bleeding.
Hemorrhoids form when abnormal connections are made between arteries and veins in the rectum.
Embolization works by blocking these abnormal blood vessel connections, which eliminates the bleeding.
Using embolization to treat hemorrhoids emerged after the first results of the technique were published in 2016.
The research supports using this procedure as a safe and highly effective treatment for hemorrhoids.
During the procedure a tiny catheter is precisely guided from an artery in the wrist or inguinal region until it reaches the superior rectal artery branches of the inferior mesenteric artery, which supplies blood to the hemorrhoids. Once the catheter is in position, embolic agents, such as small particles or coils, are injected into the artery to block the blood flow to the hemorrhoids. By blocking the blood supply to the hemorrhoidal tissue, the hemorrhoids shrink and eventually resolve. The procedure is typically performed under moderate sedation with the patient asleep. This procedure is generally considered a safe and effective treatment option for symptomatic hemorrhoids, offering a shorter recovery time and potentially fewer complications compared to traditional surgery.
Final thoughts
What to expect After Your Procedure
In the days following the procedure, it is important to take care of yourself and follow your doctor’s instructions for a smooth recovery. This may include taking medications as prescribed and avoiding strenuous physical activities or lifting heavy objects.
Most patients can return to their normal activities immediately after the procedure with some mild fevers or soreness for a few days after the procedure.
The Vascular Care Group team is here to help get you back to your favorite activities and feel like yourself again. Request an appointment today to learn more about what hemorrhoid embolization can look like for you.